Exosome Therapy in ALS: Promising Science, Experimental Treatment
Amyotrophic lateral sclerosis (ALS, or Lou Gehrig’s disease) remains a fatal neurodegenerative condition with limited treatment options. Recently, attention has turned to exosome therapy – using cell-derived extracellular vesicles (EVs) to deliver therapeutic molecules – as a novel strategy in ALS frontiersin.org. While exosome-based treatments are still highly experimental, growing evidence from preclinical research suggests they could offer neuroprotective benefits frontiersin.org. This trending update examines the potential of exosome therapy for ALS, balancing cautious optimism with current scientific evidence.
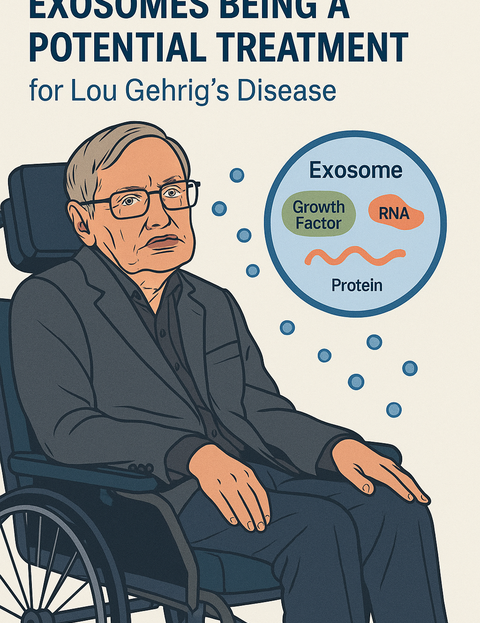
What Are Exosomes and Why ALS?
Exosomes are nanoscale vesicles released by virtually all cells, loaded with proteins, RNAs, and other signaling molecules alsnewstoday.com. Unlike whole cells or large drugs, these tiny vesicles can cross the blood–brain barrier (BBB) to deliver their cargo to the central nervous system frontiersin.org – an important advantage in treating brain and spinal cord diseases. Notably, transplanted stem cells themselves cannot easily cross the BBB, and research suggests their benefits in ALS may come largely from the healing factors they secrete via exosomes frontiersin.org. Scientists therefore hypothesize that administering purified exosomes from stem cells could replicate the cells’ neuroprotective effects by shuttling growth factors, anti-inflammatory signals, and genetic material directly to affected motor neurons pmc.ncbi.nlm.nih.gov. This cell-free approach may avoid some risks of cell transplantation while targeting hard-to-reach neural tissues.
Promising Preclinical Findings
Early studies in the lab and in animal models have yielded encouraging signs of exosomes’ therapeutic potential in ALS:
-
Neuroprotection in models: Exosomes derived from mesenchymal stem cells (MSCs) have shown the ability to protect neurons. For example, exosomes from adipose-derived MSCs reduced oxidative-stress damage in ALS model motor neurons in vitro and improved their survival by modulating apoptotic proteins pmc.ncbi.nlm.nih.gov. In ALS mouse models, the same MSC exosomes were observed to slow disease progression, corresponding with reduced inflammatory glial activation and improved motor function pmc.ncbi.nlm.nih.gov. These findings suggest exosomal cargo can favorably influence ALS pathology at the cellular level.
-
Supporting cells and vasculature: Beyond neurons, exosomes may aid other cell types involved in ALS. One study showed exosomes from human bone-marrow endothelial progenitor cells could repair ALS-related vascular damage – restoring injured brain endothelial cells exposed to toxic ALS patient factors pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov. By entering damaged endothelial cells and delivering protective signals, these exosomes significantly reduced cell death in the model. Such results hint that exosome therapy might counteract the blood–spinal cord barrier breakdown and microvascular injury seen in ALS, potentially improving the neural environment.
-
Natural delivery vehicles: Researchers are also exploring exosomes as drug delivery carriers for the brain. Because they can traverse the BBB and are biocompatible, exosomes have been used to ferry therapeutic molecules in other neurological disease models (e.g. exosome-loaded chemotherapy for brain tumors) pmc.ncbi.nlm.nih.gov. This raises the possibility of engineering exosomes to deliver drugs or gene therapies directly to motor neurons in ALS – a strategy that could overcome a major hurdle in neurodegenerative treatment (the limited brain penetration of most drugs). While this approach is still in early research, it underscores the versatility of exosomes as a platform for emerging ALS therapies.
Early Clinical Insights
Translating exosome therapy to patients has only just begun. In 2024, a first-in-human pilot study tested MSC-derived exosomes in ten ALS patients pubmed.ncbi.nlm.nih.gov. Participants received two intravenous exosome infusions a month apart. The results were encouraging in terms of safety: no serious adverse events were observed pubmed.ncbi.nlm.nih.gov. Clinically, while this small, uncontrolled study could not prove effectiveness, about 30% of patients showed no functional decline (stable ALSFRS-R score) over the 3-month follow-up pubmed.ncbi.nlm.nih.gov. This contrasts with the typical steady progression of ALS, hinting at a possible slowing of disease in some individuals. Investigators emphasized that larger controlled trials are needed to confirm any benefit, optimize dosing, and understand how exosome treatment might influence ALS long-term pubmed.ncbi.nlm.nih.gov.
Such trials are now underway. In China, a Phase 1/2 multicenter trial is evaluating intranasal administration of human umbilical cord MSC-derived exosomes in ALS patients centerwatch.com. This randomized, placebo-controlled study (launched in late 2024) aims to assess safety and preliminary efficacy of exosome nasal drops, a non-invasive route to target the brain. Similarly, a recent U.S. trial delivered an investigational exosome product (AlloEx) via nasal drops to ALS patients (NCT07105371); that early-phase study has completed enrollment and will report on safety and functional outcomes htsyndication.com. These efforts reflect a growing interest in testing exosomes in the clinic, following the positive signals from preclinical research.
Notably, industry players are also exploring exosome-based ALS treatments. BrainStorm Cell Therapeutics, developer of the MSC therapy NurOwn, has secured patents on the use of exosomes derived from its NurOwn cells for ALS and other neurodegenerative diseases alsnewstoday.com. The company is developing a distinct exosomal product intended to deliver the same neurotrophic (nerve-supporting) factors that NurOwn cells produce, but via exosomes that could reach neurons more directly alsnewstoday.com. This crossover from cell therapy to exosome therapy underlines the translational appeal – the hope that exosomes might concentrate the beneficial secretions of stem cells in a more targeted, scalable form.
Challenges and Future Outlook
Despite these advancements, experts caution that exosome therapy for ALS remains in its infancy. To date, most positive results exist only in cells and animal models; no conclusive evidence yet demonstrates that exosomes can halt or reverse ALS in patients frontiersin.org. Key questions remain unanswered – for instance, the optimal exosome dose and treatment frequency, the best route of delivery (IV infusion vs. intrathecal vs. intranasal), and how to consistently manufacture potent exosome preparations pubmed.ncbi.nlm.nih.govfrontiersin.org. Technical hurdles such as isolating pure exosomes, maintaining their stability during storage, and scaling up production to clinically relevant quantities will need to be overcome before any widespread therapeutic use frontiersin.org. There are also open questions about safety: while exosomes appear generally well-tolerated so far, careful monitoring is required to ensure no unexpected immune or off-target effects as human studies expand.
Overall, the tone in the scientific community is one of cautious optimism. Experts recognize that it is “a long way to go” before exosome therapy can become an approved ALS treatment, yet current research has brought new hope for patients frontiersin.org. Every new peer-reviewed study and early trial is helping to build the evidence base needed to validate (or refute) the approach. In the coming years, ongoing trials will reveal whether exosome-based treatments can safely slow ALS progression or improve patient outcomes. If the promise seen in the lab translates to the clinic, exosome therapy could represent a groundbreaking addition to the ALS therapeutic arsenal. For now, it remains an exciting experimental avenue – one that warrants both rigorous investigation and tempered expectations.